Herpes on the mouth, what causes it, how many days does it take to heal? Including causes, symptoms, treatment and prevention methods
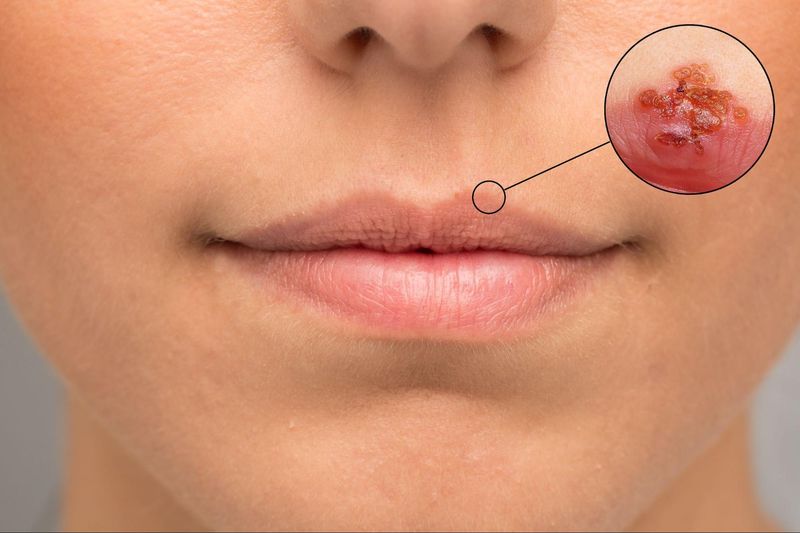
Cold sores, or oral herpes, are a common viral infection that often begins with a tingling, itching, or burning sensation around the lips. What follows is the appearance of fluid-filled blisters that can be uncomfortable, unsightly, and even distressing. While cold sores typically heal on their own, early and proper care can significantly reduce symptoms, prevent complications, and minimize the risk of recurrence.
This article provides a comprehensive guide to oral herpes—including causes, symptoms, transmission methods, stages, treatments (both medical and alternative), and preventive care. Whether you’re dealing with frequent outbreaks or simply want to understand the condition better, this guide is designed to help you manage cold sores effectively and safely.
What is Oral Herpes (Cold Sore)?
Oral herpes, commonly known as a cold sore or fever blister, is an infection caused by the Herpes Simplex Virus Type 1 (HSV-1). This condition typically results in small, fluid-filled blisters or sores appearing on the lips, the junction of the lips and the skin, or inside the mouth.
These cold sores often cause burning, itching, or pain, and may recur multiple times throughout life because the virus remains dormant in the body even after the sores have healed.
Oral Herpes Can Affect People of All Ages
Oral herpes can affect people of all genders and ages, but it is most commonly seen in teenagers and young adults. Individuals with weakened immune systems, high stress levels, insufficient sleep, or a history of exposure to the virus are more likely to experience recurrent outbreaks.
Oral Herpes vs Other Mouth Conditions
Many people confuse oral herpes with canker sores or angular cheilitis (cracked corners of the mouth). However, these are entirely different conditions with distinct causes and treatments. (See the comparison section below.)
What Causes Oral Herpes? Causes and Risk Factors
Oral herpes is caused by an infection with Herpes Simplex Virus Type 1 (HSV-1), a highly contagious virus that spreads through direct contact with infected bodily fluids such as saliva, fluid from blisters, or contaminated personal items.
How the Herpes Virus Spreads
HSV-1 can spread through various means, including:
- Kissing or skin-to-skin contact with someone who has the virus
- Sharing personal items such as drinking glasses, utensils, lip balm, or towels
- Engaging in oral sex with an infected partner
- Touching an active cold sore or blister, even if the infected person shows no symptoms
Once infected, the virus remains in the body in a dormant state and can reactivate when the immune system is weakened.
Risk Factors for Oral Herpes Flare-Ups
Several factors can trigger oral herpes outbreaks, such as:
- High stress or lack of sleep
- Weakened immune system or underlying health conditions
- Illness or having a fever
- Prolonged sun exposure or sudden weather changes
- Hormonal changes, such as menstruation
How is Oral Herpes Transmitted?
Oral herpes is a contagious infection caused by the Herpes Simplex Virus Type 1 (HSV-1), which can easily spread from person to person—even if the infected individual shows no visible symptoms.
How Oral Herpes Spreads
Oral herpes can be transmitted through:
- Direct contact with an active sore or blister
- Kissing or touching the lips of someone with the virus
- Sharing personal items such as cups, utensils, napkins, or lip balm
- Engaging in oral sex without protection with an infected partner
The virus can enter the body through mucous membranes such as the lips, mouth, or even tiny breaks in the skin. In many cases, people may carry the virus without showing any symptoms but can still spread it to others.
When is Oral Herpes Most Contagious?
Oral herpes can be contagious from the earliest warning signs—such as tingling, itching, or burning—through to the point when the sore has dried and scabbed over. The highest risk of transmission occurs when visible blisters or open sores are present.
What Are the Symptoms and Stages of Oral Herpes?
Oral herpes presents with a variety of symptoms that can be divided into distinct stages. The severity of the symptoms may depend on whether it is the first outbreak or a recurrence.
Stages of Oral Herpes Symptoms
- Stage 1: Prodrome Phase (Early Warning Signs): The affected area may feel tingly, itchy, burning, or tight around the lips or mouth. This is the body’s early signal that a cold sore is about to develop.
- Stage 2: Blister Phase: Small, fluid-filled blisters appear, often clustered together. Some people may experience pain, burning sensations, or mild fever during this phase.
- Stage 3: Ulcer Phase (Open Sore)
The blisters burst, leaving open sores that may ooze clear or yellowish fluid. This stage can be painful and is the most contagious. - Stage 4: Scabbing Phase: The sores begin to dry out, forming scabs. Itchiness, mild irritation, or tenderness may occur during healing.
- Stage 5: Healing Phase: The scabs gradually fall off, leaving healed skin without scarring. Symptoms typically resolve fully within this phase.
Additional Symptoms That May Occur
- Low-grade fever
- Muscle aches
- Swollen lymph nodes in the neck
- Fatigue and general weakness
On average, an oral herpes outbreak lasts about 7–14 days from start to complete healing.
Oral Herpes in Children: Symptoms and Care Guidelines
Oral herpes in children is relatively common, especially in young children whose immune systems are still developing. The infection is caused by the Herpes Simplex Virus Type 1 (HSV-1).
While oral herpes in children is usually not serious, it can cause significant discomfort, pain, and the risk of spreading the virus to others.
Symptoms of Oral Herpes in Children
- Low-grade or high fever in the early stage
- Irritability and general discomfort
- Fluid-filled blisters or sores around the lips, on the lips, or inside the mouth
- Swollen lymph nodes in the neck
- Poor appetite or refusal to eat and drink due to mouth pain
In some cases, symptoms may become more severe, with higher fever, extensive mouth sores, and swollen glands.
How to Care for a Child with Oral Herpes
- Ensure the child gets plenty of rest and stays well-hydrated
- Avoid giving spicy, hot, or acidic foods that can irritate the sores
- Clean the affected area or have the child rinse with saline solution
- Use medication as advised by a doctor or pharmacist, such as antiviral drugs or fever reducers
- Avoid kissing or sharing personal items until the sores have fully healed
If the child experiences high fever, extreme fatigue, or is unable to eat or drink, medical attention should be sought immediately.
Can Stress or Allergies Cause Oral Herpes?
Many people wonder whether stress or allergies can cause oral herpes. The answer is that stress and a weakened immune system are common triggers for cold sore outbreaks, but they are not the primary cause of infection.
How Does Stress Affect Oral Herpes?
- When the body experiences stress, the hormone cortisol increases, which can weaken the immune system.
- A weakened immune system allows the Herpes Simplex Virus (HSV-1)—which remains dormant in the body—to reactivate and cause cold sores.
- Outbreaks often occur during periods of emotional stress, lack of sleep, or physical exhaustion.
Do Allergies Cause Oral Herpes?
- Allergies themselves do not directly cause oral herpes.
- However, severe allergic reactions—such as skin inflammation, rashes, or cracked lips—may create openings in the skin or mucosa that allow the virus to enter or flare up more easily.
In conclusion, while stress and allergies are not direct causes of oral herpes, they can significantly increase the likelihood of a recurrence. Managing stress and maintaining good skin care can help reduce the frequency of outbreaks.
Is Oral Herpes Dangerous? Potential Complications to Watch For
In most cases, oral herpes is not a serious illness and typically heals on its own within 1–2 weeks. However, certain individuals—especially those with weakened immune systems or underlying health conditions—may be at risk of more serious complications.
Possible Complications of Oral Herpes
- Secondary Bacterial Infection Open cold sores can become infected with bacteria, leading to redness, swelling, and possible pus formation.
- Spread to Other Parts of the Body Touching a cold sore and then touching the eyes may cause ocular herpes (Herpes Simplex Keratitis), which can be severe and potentially lead to vision loss if untreated.
- Herpes Encephalitis (Brain Infection) Although very rare, the herpes virus can spread to the brain, causing high fever, severe headache, seizures, or unconsciousness.
- Chronic Herpes in Immunocompromised Individuals People with weakened immune systems—such as those with HIV or cancer—may experience more severe, long-lasting, or recurring outbreaks.
Who Is at Higher Risk for Complications?
- Individuals with weakened immune systems
- Those undergoing chemotherapy or taking immunosuppressive drugs
- People living with HIV/AIDS
- Infants and young children
If you or someone you know develops severe symptoms such as high fever, persistent headache, seizures, or cold sores that do not improve within 10 days, medical attention should be sought immediately.
Can You Have Oral Herpes Without Blisters?
While visible blisters or cold sores are the most common symptom of oral herpes, it is entirely possible to be infected without developing any visible sores—especially during the initial infection or in mild recurrent episodes.
Why Oral Herpes Might Not Show Blisters
- Some individuals have immune systems that suppress the virus effectively, resulting in very mild or unnoticed symptoms.
- A flare-up may only involve tingling, burning, or itching around the lips without any visible blister.
- The virus can remain dormant in the body for years without causing visible outbreaks (asymptomatic infection).
Signs to Watch For—Even Without Blisters
- Recurring tingling or sensitivity around the lips
- Past history of cold sores or exposure to someone with oral herpes
- Occasional burning sensations without visible sores
- Episodes triggered by stress, lack of sleep, or hormonal changes
If you suspect you have oral herpes but do not have visible symptoms, consult a healthcare professional. A blood test for HSV antibodies or a clinical assessment may help confirm the diagnosis.
How to Treat Oral Herpes: What Works and What Medications Help?
In most mild cases, oral herpes can heal on its own. However, proper treatment can help speed up recovery, reduce symptoms, lower the risk of transmission, and prevent frequent recurrences.
Treatment Options for Oral Herpes
- At-Home Care Tips
- Get plenty of rest and stay hydrated
- Apply a cold compress to the affected area to reduce swelling and discomfort
- Avoid spicy, salty, hot, or acidic foods
- Rinse your mouth with saline water if there are sores inside the mouth
- Antiviral Medications: Antiviral drugs are most effective when taken at the first sign of symptoms, such as tingling or burning sensations.
Common medications include:- Acyclovir
- Valacyclovir
- Famciclovir
- These are available in both oral and topical forms, and should be used under the guidance of a doctor or pharmacist.
When to See a Doctor
- If symptoms are severe or blisters are spreading rapidly
- If outbreaks occur frequently (more than 6 times per year)
- If you have a weakened immune system (e.g., HIV)
- If the patient is a child or elderly person with unusual symptoms
Herbal Remedies for Oral Herpes: What Works and Is It Safe?
While antiviral medication remains the primary treatment for oral herpes, some individuals opt for herbal remedies to help relieve symptoms. However, herbal treatments should always be used cautiously and under professional guidance to ensure safety and effectiveness.
Common Herbal Remedies for Cold Sores
- Clinacanthus nutans (also known as “Phaya Yor”): This Thai herb has anti-inflammatory properties that may reduce burning and promote faster healing.
It is available as topical creams or gels and should only be applied externally to the affected area. - Aloe Vera: Aloe gel helps moisturize the lips, soothe irritation, and reduce inflammation. It is gentle and commonly used for skin care.
- Betel Leaf / Andrographis (Fah Talai Jone): These herbs have antibacterial and anti-inflammatory effects, but should be used with caution around the mouth.
Tips for Safe Herbal Use
- Choose products that are registered with national health authorities (e.g., FDA or equivalent)
- Apply only externally, never inside the mouth
- Stop use immediately if any allergic reaction or irritation occurs
- Avoid combining herbal remedies with other treatments unless advised by a doctor or pharmacist
While herbal remedies may provide symptom relief, they should not replace prescribed antiviral medications. If symptoms persist for more than 5–7 days, medical advice is strongly recommended.
How Long Does Oral Herpes Last? How to Heal Faster
Cold sores caused by oral herpes usually resolve on their own within 7–14 days. However, the healing time may vary depending on individual immunity, general health, and how well the sore is cared for.
Cold Sore Healing Timeline
- Days 1–2: Tingling, itching, or burning sensation begins around the lips
- Days 3–5: Small blisters form and eventually burst, becoming open sores
- Days 6–10: Sores begin to dry out and scab over
- Days 11–14: Scabs fall off and the skin heals, usually without scarring
For individuals with weakened immunity or poor self-care, healing may take longer.
Tips to Heal Faster
- Start antiviral treatment immediately at the first sign of symptoms (tingling or burning)
- Avoid touching, scratching, or picking at the sores to prevent further irritation or infection
- Get adequate rest and manage stress to support your immune system
- Eat a balanced diet rich in lysine (e.g., fish, eggs, legumes)
- Avoid spicy, acidic, or fermented foods that might trigger flare-ups
Proper care can speed up recovery and help prevent future outbreaks.
Can You Have Sex While Having Oral Herpes? What Are the Risks?
A common concern is whether it’s safe to engage in sexual activity while having oral herpes. The answer is: it’s possible, but carries a high risk of virus transmission, especially if not properly protected or if symptoms are present.
Can Oral Herpes Be Transmitted Through Sex?
- Oral herpes is caused by Herpes Simplex Virus type 1 (HSV-1): It can be transmitted through kissing or oral sex even when sores are not visible
- Performing oral sex during an outbreak or even during asymptomatic periods can transmit HSV-1 to a partner’s genitals
- This may result in genital herpes caused by HSV-1
How to Reduce the Risk During Sexual Activity
- Avoid all forms of sex (including oral) during outbreaks or when tingling/burning is present
- Use condoms or dental dams consistently during oral or penetrative sex
- Disclose your herpes history to partners to assess the risk together
- In high-risk cases, consult a doctor about PEP or PrEP to reduce the chance of HIV infection if open sores are present
Remember: even without symptoms, those with a history of herpes may still shed the virus and infect partners without knowing.
How Is Oral Herpes Transmitted? Do You Need to Isolate?
Oral herpes is highly contagious, especially during outbreaks when cold sores or blisters are visible. Understanding how it spreads is key to preventing transmission—particularly in close-contact environments like home or work.
How Is Oral Herpes Spread?
- Direct contact with cold sores or fluid-filled blisters—e.g., kissing or oral sex
- Sharing personal items such as drinking glasses, utensils, towels, lip balm, or toothbrushes
- Asymptomatic shedding: Even without visible symptoms, the virus can still be transmitted
Do You Need to Isolate?
Generally, oral herpes does not require full isolation like severe contagious diseases. However, extra caution is recommended during outbreaks.
Tips to Prevent Spreading the Virus
- Avoid kissing, facial contact, or sharing items with others
- Refrain from oral sex or activities involving mouth-to-skin contact
- Wash hands frequently and avoid touching the cold sore
- Avoid close contact with infants, young children, or immunocompromised individuals
If you work closely with others or care for vulnerable people, consult a healthcare provider before returning to regular duties.
What’s the Difference Between Oral Herpes and Genital Herpes?
Many people wonder whether oral herpes and genital herpes are the same disease. While they’re both caused by the Herpes Simplex Virus (HSV), they differ in the type of virus, site of infection, and mode of transmission.
Types of Herpes Virus
- Oral herpes is typically caused by HSV-1
- Spread through kissing, sharing items, or oral sex
- Genital herpes is usually caused by HSV-2
- Transmitted through penetrative sex or genital contact
However, HSV-1 can also cause genital herpes—especially through oral-genital contact.
Key Differences Between Oral and Genital Herpes
|
Comparison Point |
Oral Herpes (HSV-1) |
Genital Herpes (HSV-2) |
|---|---|---|
|
Infection Site |
Lips, mouth, facial areas |
Genitals, anus, buttocks |
|
Symptoms |
Tingling, itching, blisters |
Painful blisters, swelling, fever |
|
Transmission Methods |
Kissing, oral sex, shared items |
Sexual intercourse, oral sex |
|
Recurrence Frequency |
Less frequent |
More frequent |
|
Potential Complications |
Usually mild |
May affect pregnancy in some cases |
Should You Get Tested for HSV Type?
If you’ve had herpes before and experience new symptoms or suspect a different infection site, consider blood testing or PCR to confirm the HSV type. This helps guide treatment and prevention for your partner.
Is Oral Herpes Related to HIV? How High Is the Risk?
While oral herpes and HIV are caused by different viruses, they are indirectly linked, particularly in terms of increased HIV transmission risk when cold sore lesions are present.
How Can Oral Herpes Increase HIV Risk?
- Cold sores create open wounds on the lips or in the mouth, making it easier for HIV to enter the body during exposure
- Engaging in oral sex while having cold sores, especially with an HIV-positive partner, significantly raises the risk of transmission
- Frequent outbreaks of herpes may indicate a weakened immune system, which could be a sign of or contribute to other underlying infections
What Should You Do If You’re Worried About HIV?
- If you’ve had a recent high-risk exposure, such as unprotected oral sex during an outbreak, consider taking PEP (Post-Exposure Prophylaxis) within 72 hours
- For ongoing high-risk behavior, talk to a doctor about PrEP (Pre-Exposure Prophylaxis) to reduce your long-term risk of contracting HIV
HIV testing and counseling are available at specialized clinics like Safe Clinic, and early prevention makes a big difference in long-term health.
Frequent Cold Sores (More Than 6 Times a Year): What Does It Mean? How to Manage It?
Experiencing cold sores more than six times per year is considered unusually frequent and may indicate an underlying immune issue or chronic health concern that needs attention.
What Could Frequent Oral Herpes Indicate?
- Weakened immune system: Often due to chronic stress, lack of sleep, or illness
- Chronic health conditions: Such as diabetes, malnutrition, or HIV
- Long-term use of immunosuppressive drugs or corticosteroids
If other symptoms are present—like fatigue, weight loss, or slow wound healing—consult a doctor for further evaluation.
How Is Chronic Oral Herpes Treated?
- Suppressive therapy: Involves daily antiviral medication to reduce the frequency of outbreaks
- Common drugs include Acyclovir, Valacyclovir, and Famciclovir
- Boost immune health: Through regular sleep, exercise, stress management, and a nutritious diet
- Medical follow-up: With a specialist to rule out or manage any underlying conditions
Frequent outbreaks warrant medical evaluation to identify root causes and develop a personalized long-term treatment plan.
Should You Pop a Cold Sore Blister?
It’s common to feel tempted to pop or pick a cold sore blister, thinking it might heal faster. However, from a medical standpoint, you should never pop a cold sore. Doing so can increase the risk of complications and further spread of the virus.
Why You Shouldn’t Pop Cold Sores
- Risk of secondary infection: Breaking the skin can allow bacteria to enter, leading to further infection
- Higher chance of spreading the virus: The fluid inside cold sores contains a high concentration of the herpes virus and can easily spread to other parts of your body—or to others
- Slower healing time: Popping or picking at the sore may make it worse, causing deeper wounds and longer recovery
How to Properly Care for a Cold Sore
- Avoid touching, scratching, or popping the blister
- Use topical or oral antiviral medication as prescribed by a doctor
- Gently cleanse the area with saline or boiled water using a clean cloth
- Wash your hands regularly and avoid unnecessary contact with the sore
If the sore becomes very painful, filled with pus, or is accompanied by a fever, seek medical attention for proper evaluation and treatment.
Oral Herpes in Children and Infants: Is It Dangerous? How to Care for It
While oral herpes in adults is usually mild, it can be more serious in infants and young children due to their immature immune systems. Special care and early medical attention are essential.
Why Is Oral Herpes More Dangerous in Children?
- In infants, HSV-1 can potentially spread to the brain or meninges, leading to herpes encephalitis, which can be life-threatening
- Symptoms may include high fever, vomiting, seizures, lethargy, or refusal to eat
- In newborns, herpes can become a systemic infection (disseminated herpes), affecting multiple organs
Symptoms of Oral Herpes in Children and Infants
- Blisters or sores around the mouth or lips, swollen red gums
- Excessive drooling, pain while eating, or refusal to breastfeed
- Irritability, fever, drowsiness, and sometimes spreading rash or blisters
How to Care for a Child With Oral Herpes
- Seek pediatric medical attention immediately, especially for babies under 6 months old or with high fever
- Do not pop blisters or apply any creams or ointments without a doctor’s advice
- If confirmed by a doctor, antiviral medication may be prescribed orally or intravenously
- Clean the mouth area gently with warm water and ensure the child stays well-hydrated
Prevention is critical—adults with visible cold sores should avoid kissing or close contact with infants during outbreaks.
Conclusion
Although cold sores are often viewed as minor or harmless, they can have a meaningful impact on your quality of life—especially if left untreated or if they recur frequently. In certain individuals, such as infants, elderly patients, or those with weakened immune systems, herpes infections may lead to serious complications.
Understanding the triggers, recognizing symptoms early, and knowing how to treat and prevent oral herpes are key to reducing discomfort and transmission. If you experience frequent outbreaks or have concerns about your symptoms, consult a healthcare professional to receive personalized guidance and care.





